Finger pricks and continuous glucose monitors may be things of the past if A&M researchers succeed in developing a new way to measure a diabetic’s glucose levels through fluorescent light.
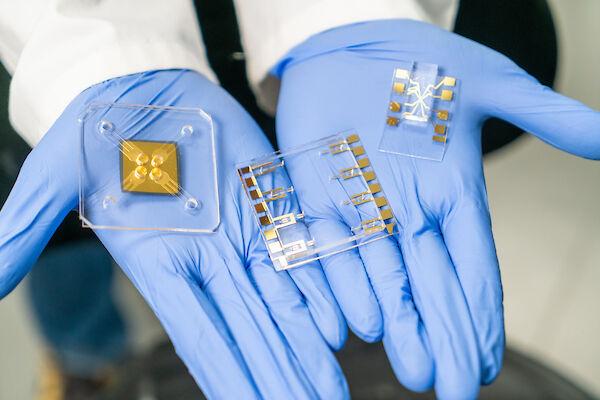
Two research labs aim to develop a device the size of a rice grain that can be implanted in the skin and will glow certain colors when fluorescent light is shined upon it. The colors will correspond to the diabetic’s glucose level, allowing an individual to monitor their health without the invasive, and sometimes painful, procedures available today.
Heading the labs that seek to develop this device is Gerard Cote, director of the Center for Remote Healthcare Technology, and Melissa Grunlan, director of undergraduate programs in the Department of Biomedical Engineering.
“We are working on a device that you can implant just underneath the skin that will change its color or its fluorescence, if you will, with changes in glucose concentration,” Cote said.
When the device is implanted under the skin, it is probed by shining a certain color of light on it. The person using the implant can painlessly and unobtrusively correlate the color changes with their blood sugar level.
This would provide a way for diabetics to continuously and noninvasively measure their blood glucose. The device’s design is a joint project between Cote’s and Grunlan’s labs.
Diabetes is a demanding disease to deal with. Individuals with diabetes sometimes have to prick their finger or forearm at least four or five times a day to monitor sugar levels. They must always be aware of their blood sugar, because if it gets too low they can become light-headed, shaky and may even risk a coma or death.
The finger-prick method has several disadvantages compared to the device Cote and his team are developing.
“When you prick your finger, you open it up for infection, and quite frankly it’s embarrassing for some people to pull out their meter when they have to monitor their sugar, say out at a restaurant,” Cote said.
The other way blood sugar is monitored is called continuous glucose monitoring, during which a patient will stick the needle of a device into his or her stomach area. This device sends data to a meter that provides constant glucose levels, but it has several downsides.
“It is indwelling,” Cote said. “It is sticking out of the skin just like an insulin pump does and it is very uncomfortable. Also it must be calibrated against the finger prick device once a day. These devices must be pulled out and switched every three to seven days.”
Cote and his team aim to fix these problems by implementing a small device the size of a rice grain underneath the skin. Once it is implemented, doctors allow the skin to heal over it and glucose can be easily and noninvasively monitored for at least three months to a year before it needs replacing. Users must simply shine a fluorescent light from a watch or other device to get a reading.
Andrea Locke, a doctoral student in Cote’s lab, said the lab works with the chemistry that uses glucose to produce fluorescence while Grunlan’s lab works on the biocompatible membrane that will hold the assay, or the molecule that interacts with the glucose to determine what color the device will show.
The device uses two fluorescent dyes — one is tied to a protein that binds to glucose, and the other is tied to a sugar that competes for the binding site on the protein.
Although the process sounds complicated, it is actually quite simple, Locke said.
“When no glucose is in the blood, these dyes will be in close proximity to each other and the second dye will give off fluorescence,” Locke said. “But when there is more glucose in the bloodstream, the distance between the dyes increases and the first dye fluoresces intensely while the second is minimized.”
The project is advancing, but it still has some obstacles to overcome. Locke said while the assay performs well in a free solution, it has trouble when placed in the capsule the team hopes will eventually hold it. Cote said another issue is determining how long the device can remain in the body before the chemistry on which it is based stops working.
The biocompatibility, or how well the body accepts the device, is the final hurdle.
“The body does one of three things when it is injected with something,” Cote said. “The first thing the body will try is to push the foreign object out, like a splinter. If the body can’t push it out it tries to eat it up, and dispose of it. If the body can’t do either of these, it tries to put a capsule around it to protect the rest of the body.”
Any of these would render the device useless, so Grunlan’s lab is designing a material that shrinks and swells to combat the encapsulation.
The implants still need to go through several phases of human and animal testing that will take several more years before it can start being used clinically.
A&M diabetes research could end painful insulin tests
April 19, 2015
Donate to The Battalion
Your donation will support the student journalists of Texas A&M University - College Station. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.