For the past two decades, D. Samba Reddy, professor of neuroscience and experimental therapeutics at the Texas A&M College of Medicine, has been searching for answers to catamenial epilepsy, a subset of chronic epilepsy that causes a dramatic increase in seizures during a women’s menstrual periods.
Although this condition has been documented for millennia, there is currently no effective treatment for catamenial seizures, leaving many women and their families desperate for answers.
Reddy said he frequently receives emails from women around the world, pleading for his help, as his research has been pivotal in cracking the basic neural code underlying catamenial epilepsy and mobilizing resources for researching this female-specific brain condition.
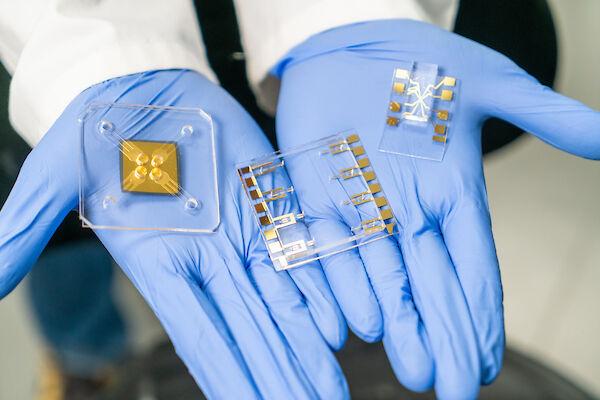
After piecing together hormone mechanisms, specific models and therapeutic strategies in sequential projects, Reddy has published a report in the October 2017 issue of the Journal of Neuroscience Research. The paper, co-authored by his doctoral student Bryan Clossen, is the first of its kind to use modern transgenic tools to investigate the age-old problem of hormonal seizures in women with epilepsy.
“Normal antiepileptic drugs don’t work for these patients,” Reddy said. “For a long time, doctors have been treating women with catamenial epilepsy the same way that they would treat men with epilepsy.”
Reddy said these methods do not act the same on males and females.
“This is ineffective, because the hormonal changes that occur during the menstrual cycle make the brain insensitive to typical epilepsy medications like diazepam and valproate,” Reddy said.
During a woman’s menstrual cycle, there are four separate phases that occur sequentially: The follicular, ovulatory, luteal and menstruation phases. These phases affect the ratio of the hormones estrogen and progesterone in the blood serum, which affect the level of excitation in the brain. This leads to catamenial seizures in many women with epilepsy. An estimated 300,000 to 500,000 Americans experience catamenial epilepsy.
“If a brain with epilepsy is too excited, then its electrical circuits will misfire excessively and cause the person to have a seizure,” Reddy said. “However, if someone with epilepsy keeps a high level of tonic inhibition in the brain, the electrical circuits do not get overexcited and a seizure will not occur.”
Neurosteroids play an important role in balancing neuronal excitability by making brain receptors either more or less responsive to the neurotransmitters that mediate tonic inhibition. When the hormone progesterone is released in the body, it travels to the brain and is converted into a neurosteroid known as allopregnanolone.
“Allopregnanolone preferentially binds to a type of receptor in the brain and makes these receptors more responsive to the neurotransmitter gamma-aminobutyric acid, also known as GABA,” Reddy said.
GABA functions as an inhibitory neurotransmitter in the brain, so it is critical for individuals with chronic epilepsy. When a lot of GABA binds to GABA receptors in the brain, the electrical circuit in the brain is able to remain inhibited so that a seizure does not occur. This means that the presence of progesterone in the blood is critical to keeping seizure levels low in women with catamenial epilepsy.
Essentially, when progesterone levels decrease, such as during menstrual periods, it causes allopregnanolone levels to decrease, which results in extrasynaptic receptors being less sensitive to GABA, which results in increased excitation in the brain. This leads to an increase in the number of seizures for women with catamenial epilepsy.
“When it comes to the menstrual phase in the cycle, the tonic inhibition in the brain vanishes because there is very little neurosteroid being produced,” Reddy said. “As a result, the inhibition levels are reduced and the circuits become hyper-excitable.”
In this study, the researchers examined the impact of decreased levels of neurosteroids in the hippocampus, an area in the brain that regulates seizure circuits.
They removed the extrasynaptic delta GABA-A receptors that mediate tonic, or sustained, inhibition in the brain to check the hippocampal vulnerability to seizures. Then the menstrual cycle was simulated by fluctuating circulating levels of neurosteroids like allopregnanolone. Their results showed a significant increase in the severity and duration of seizures when there were low neurosteroid levels.
“We cracked the neuronal code of tonic inhibition, the electrical circuit shunting force mediated by extrasynaptic delta GABA-A receptors in the hippocampus, as the major regulator of the catamenial seizures,” Reddy said. “This opens up the possibility to start clinical trials that focus on treating catamenial epilepsy with synthetic neurosteroid agents that enhance tonic inhibition.”
The paper’s findings hint at a platform for clinical trials to translate the research from bench to bedside. A pulse therapy with low doses of neurosteroid agents may help control catamenial seizures without side effects.
“I stumbled across your website while doing a google search for my wife’s illness,” a patient said in an email to Reddy. “You are doing amazing research and I hope human clinical trials will be coming soon. I truly believe my wife and thousands of others could benefit from your research.”
The process of developing a cure for catamenial epilepsy is far from over. Reddy, through his relentless research for over 20 years, has been continuously funded by the National Institutes of Health for over 13 years.
Editor’s Note: Sarah Elmer contributed to the writing of this article. This article originally ran in Vital Record and has been edited to fit AP Style.