Editor’s Note: ‘John’ and ‘Joan’ are pseudonyms to protect the source’s identities.
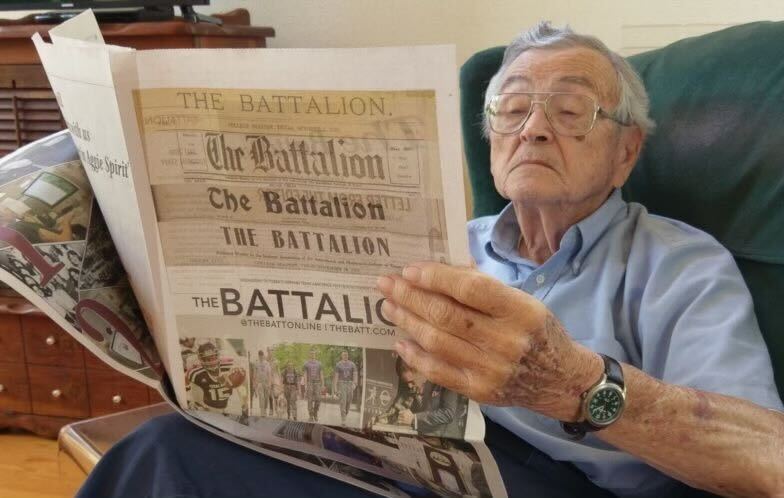
John is no stranger to the stillness behind closed doors. In the course of his everyday routine, John passes by a terrain of wrinkled faces, a sea of loosening jowls and an unpredictable atmosphere sporadically pierced with violent yells of deeply disturbed patients. Joan rarely says much when her husband John visits. Still, John has learned to communicate with his wife more in silence than frivolous banter. His gaze often shifts from his sleeping wife to her drip-feed to her plush tiger, which usually lit a fiery sparkle in Joan’s eyes.
In December 2019, Joan suffered three crippling strokes that forced John to commit his wife to a long-term rehabilitation care facility. In early March of the following year, she was doing well, and John was looking forward to bringing his wife back home.
However, things took a turn for the worse when COVID-19 entered the picture. The pandemic outbreak revealed a critical void in our approach to caring for the vulnerable. With the sterile, clinical atmosphere of most care homes and the unmistakable stench of stale urine, it is easy to point the finger at these “homes.” It is also easy to condemn in such a detached and frozen land the icy workers, who are undeterred by the fading memories of the once bright patients.
But are they to be blamed for cold demeanors when juggling the impossible components of a broken system? They have to care for their patients, communicate with their families and still follow the rules and protocols about healthcare and its financing, often set by bureaucrats and businessmen in cozy boardrooms, unconcerned about hard realities on the ground.
Long-term care has always been plagued with underinvestment, understaffing and low-wage workers.
“Staffing is the biggest problem. There’s no way around it,” John said. “They don’t pay the staff to get high-quality care. The ones they do have, they push too hard on.”
Despite the government’s lack of backing or support, structural weaknesses have always been a breeding ground for pandemics like COVID-19. According to The Atlantic, “For years, many people in medicine have understood that late-life care for the chronically sick is not only expensive but also, much too often, ineffective and inhumane.”
Because of the lockdown, John had lost complete access to his wife. Not knowing Joan’s current condition, John’s calls to the care facility went unanswered.
“[Joan] is not physically or mentally capable of dealing with calling by herself. I had to call the nursing station and get them to turn on the phone so that I can talk to her,” John said.
Before the pandemic ravaged the world, the nursing station was doing just that — and John always had a line of connection with Joan through her personalized dial phone. But, after COVID-19 forced all nursing and rehabilitation homes to close their doors to the outside world, John’s connection to Joan was wholly cut off and disconnected.
“Sometimes I would get an answer and be told, ‘We’ll call you right back on the phone.’ Most days I’d be calling several times a day when I finally would get somebody to get her on the phone,” John said.
Answering calls is by no means beyond the call of duty for a care facility, so when the nursing station went completely radio-silent for an entire week, John grew alarmed. It was not until he threatened to report a wellness check and get the police involved did the staff finally hear him. However, when John eventually reached his wife, he realized something was really wrong.
“Within three minutes of speaking to her, I could tell she was having another stroke,” John said.
The nurse in charge, however, did not seem concerned. Believing John was on the wrong side of the line, the nurse argued with John about whether his wife was having a stroke.
“I was informed that I didn’t know what I was talking about,” John said.
Unfortunately, John’s fears were valid and the effects of this stroke, Joan’s fourth, left her completely debilitated.
“[On] her left side, neglect is complete. She has no control over the left side. [Joan] is not paralyzed, but she can’t mentally control that point,” John said.
As the second wave of COVID-19 pummeled the nursing home, John said the facility’s management was left floundering again.
“The second wave of COVID[-19] hit the nursing home. That one was bad,” John said. “Basically, the state came in and shut down. All staff was removed from the site.”
In the wake of the wreckage, loved ones like John witnessed the debris and tangled mess left behind. Since Joan had returned from the hospital, she was in complete isolation.
“They would not allow [Joan] to have any of her stuff … she was sitting in a room with no TV, no radio, no stimulation whatsoever,” John said.
Amid the chaos of trying to keep up daily functions, Joan had severe effects as the result of the staff overlooking her care. With a short staff, restorative physical therapy for Joan had screeched to a sudden halt.
“When I got to [Joan] on January 15 … her arm was trapped in this position,” John said, tucking his arm unnaturally beneath him. “The muscles were locked, solid. [Joan’s] left heel was underneath her crotch, and those muscles were locked in solid.”
John took it upon himself to help Joan with physical rehabilitation. John explained that Joan’s lack of physical therapy was likely a result of the dwindling staff.
“Since that time, every day, I worked with her on physical therapy, trying to undo it. I’ve gotten her arm to where it’ll open to about 130 degrees … but [Joan] has no spring on that side at all, stuck in contraction,” John said.
Unfortunately, he could not provide a personal physical therapist for his wife because of the stringent COVID-19 protocols and his insurance company’s unwillingness to help. Insurance issues tend to rear their ugly head in an already chaotic system with the aggrandized costliness of long-term care facilities. Addressing these financial gridlocks is like keeping down a relentless stream of moles in a futile game of whack-a-mole. Luckily, this is when an ombudsman, a government-appointed advocate, can come into play.
As the supervisor for the Ombudsman Program for the Brazos Valley Council of Governments, Angela Allison is an advocate for those in local assisted living facilities. Allison and the Ombudsman Program work on ensuring the quality of care and life in these types of facilities.
“One way that an ombudsman’s work often intersects with Medicare and Medicaid is our educational outreach where we talk to residents about their right to turn in those applications and the facility staff’s responsibility to help residents who request assistance with those applications,” Allison said.
As the only full-time staff, Allison supervises the work of 12 certified volunteers. The group oversees about 42 nursing homes and living facilities in the Brazos Valley. Despite the staff’s stress of having to meet demand, Allison remains optimistic and undeterred in her mission to help others.
“It’s definitely a challenge to have such a small staff for so many facilities but, you know, we’re always looking for more volunteers,” Allison said. “It is a lot of work. But it’s rewarding work, so I enjoy doing it.
“It can be difficult to persuade medical staff to think outside of the box, but I like that challenge. I’m trying to help them think through interesting and creative new ways to approach a resident’s needs for care.”
Nurses and caretakers are the backbone of the medical industry, and with little support and compensation from the government, we can not fault them for staggering under that weight.
Those hiding behind the rhetoric of bureaucracy and choosing to remain silent are only adding more burden than relieving it.
Unfortunately, crises such as the pandemic have made it far too easy to clump the elderly into a faceless mass — regarded more like an inescapable albatross than complex, titular individuals. With this outlook, care facilities disregard the lives of the feeble, not really as lives, but as a long sentence to wait out the clock. Nursing and rehabilitation homes should be a vibrant community filled with loving support and even more loving people — a home. Home is supposed to be a place where individuals come to live — not come to die.
If you are interested in helping to give a much-needed voice to the most vulnerable, consider joining the Ombudsman Program of the Brazos Valley.
Neha Gopal is a university studies junior and an opinion writer for The Battalion.