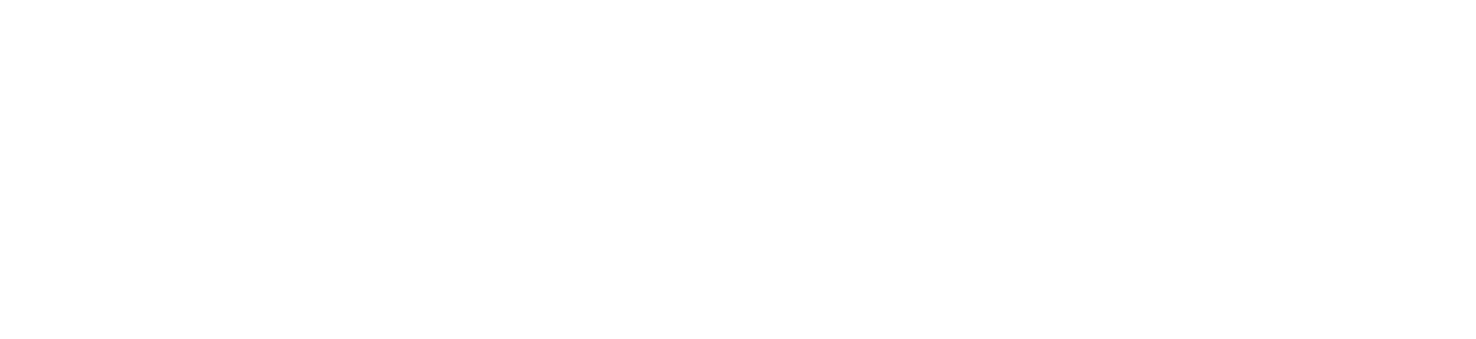
Aggies are coming together to research a strain of E. coli bacteria that can be used to combat antibiotic-resistant urinary tract infections, or UTIs. The research began in Subash Lab in the Department of Veterinary Pathobiology in 2021, and the treatment began animal testing this year.
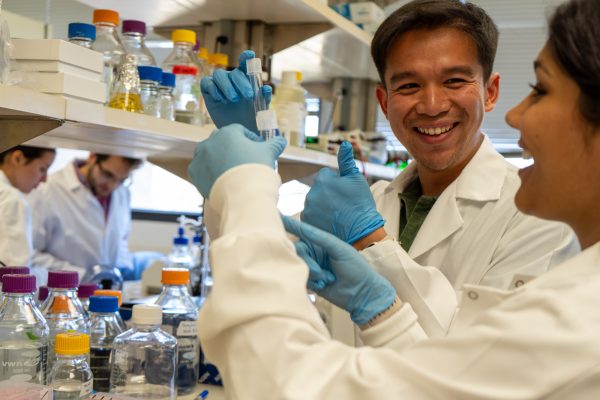
“This project started as a collaboration between my team and Dr. Taylor Ware’s team at biomedical engineering,” veterinarian and principal investigator of the project, Saguru Subash, Ph.D., said. “Outside of A&M, we have a collaborator from UT Southwestern, Dr. Phillippe Zimmun — he’s a clinical urologist, so he sees a lot of patients with recurring UTIs, and it really helps us get a clinical perspective.”
UTIs are one of the most common diseases and affect more than 150 million people worldwide every year. Most UTIs are non-threatening and easily treatable, but if left untreated, the infection can cause severe damage to the kidneys, reproductive organs and other parts of the urinary system. This becomes a bigger issue when patients with recurring UTIs become resistant to antibiotic treatment.
“Antibiotics are effective for a lot of people, but there are a large number of people who don’t respond to antibiotic therapy,” Subash said. “It never is a long term solution for a lot of people, so we wanted to look at other natural ways to combat this infectious disease.”
E. coli is typically not associated with urinary problems, and it usually carries a heavily negative connotation because the most well-known strain causes severe illnesses. Both helpful and harmful strains occur naturally in the bladder, however. Most UTIs are caused by pathogenic E. coli — but one beneficial strain combats this harmful counterpart.
“Typically, the number that is published is that 75% of UTIs are caused by E. coli,” Subash said. “A lot of times when we think of bacteria or microbes, we tend to associate them with diseases and plague and other bad outcomes, but most microbes either don’t do anything, or … they actually do a lot to benefit us.”
The combative strain was discovered 50 years ago in Sweden and is already used as a preventative measure throughout Europe, according to veterinary biomedical sciences graduate student Iris George. Determining exactly how the strain — named the asymptomatic bacteriuria strain, or ABU — combats UTIs is George’s project.
Subash and George both said that the foundational research is long-standing and has been a helpful starting point, but to use this discovery as treatment, they need to better understand how the bacteria works.
“This ABU strain can compete with uropathogens, so I’m [studying] how they are competing,” George said. “After knowing what the mechanism is, we can find more innovative works and alternative approaches against UTIs.”
Researchers have discovered that the beneficial bacteria compete against the harmful E. coli by starving pathogens of the specific nutrients it needs. However, they are still working to find ways to turn this bacteria into a treatment.
“One of the major limitations of this strain is that it doesn’t colonize people very well,” Subash said. “So even if you instill it in the bladder, it tends to get lost unless you have a bladder pathology which allows excessive urine to always remain in the bladder — then the strain will grow fine.”
The biomedical engineering team has developed hydrogels that trap the beneficial E. coli bacteria so it can be slowly released over time to compete with pathogens. This delivery method is currently being tested on a mouse model and could be potentially used in human treatments as well.
“What we are realizing is that this bacteria has to be present when the pathogens are there,” Subash said. “ … So because of the mechanism of competition, we have to get this bacteria locally in the bladder and not necessarily through an oral medication.”
The testing phase of these hydrogel treatments is still in its infancy, but Subash hopes this good bacteria can be used as a treatment for humans in the near future.
“This is pure speculation because we clearly don’t know how this will work out in lab animals, in actual animals and then humans, [but] I think in the best possible scenario we’re looking at like five to seven years,” Subash said.